We are a complex society that (also) evolved thanks to our communication abilities. However, if communication is difficult or impossible, the consequences can be devastating, as we have seen during the management of the COVID-19 pandemic. We were not really prepared in that case, or we have over-estimated our preparation, but at least we might have learned some lessons (see this paper, for instance). In this The Lancet piece of 2022 lessons for the future have been outlined: and unfortunately the future seems to be closer than ever, nowadays.
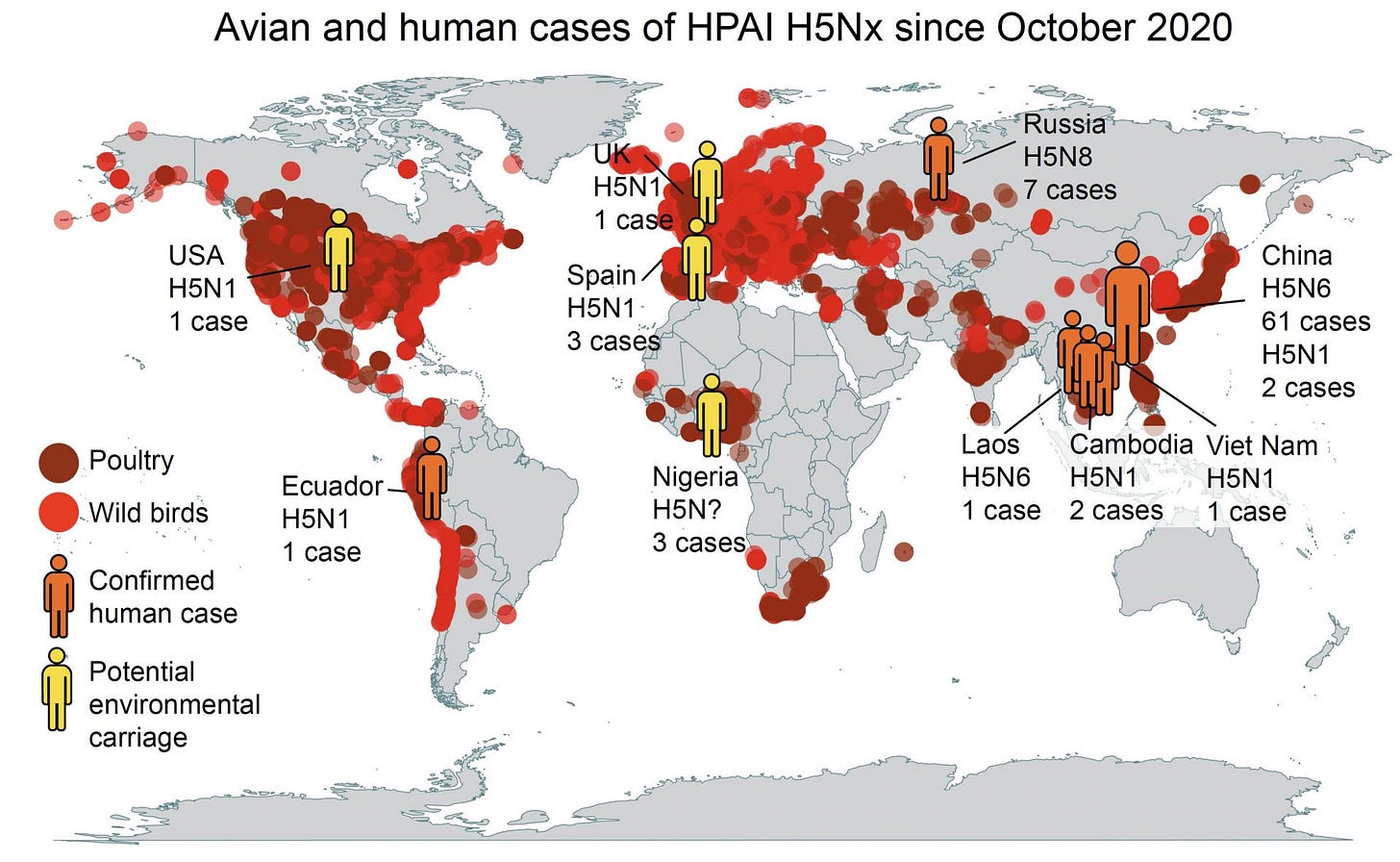
The global health is being shaken again by the emergence of two non-negligible threats: avian influenza, that is increasingly adapting to mammals (→ CDC on dairy cows), and the recent World Health Organization’s (WHO) declaration of mpox (formerly known as monkeypox) as a Public Health Emergency of International Concern (PHEIC, → WHO declaration). These events have raised alarms not only within the scientific community but also among policymakers and the general public, especially because we are still learning to co-exist with the SARS-CoV-2, the virus responsible for the COVID-19 pandemic. While each of these health threats is significant on its own, their simultaneous emergence highlights the complex interplay between human activity, environmental and ecological change, and epidemic dynamics.
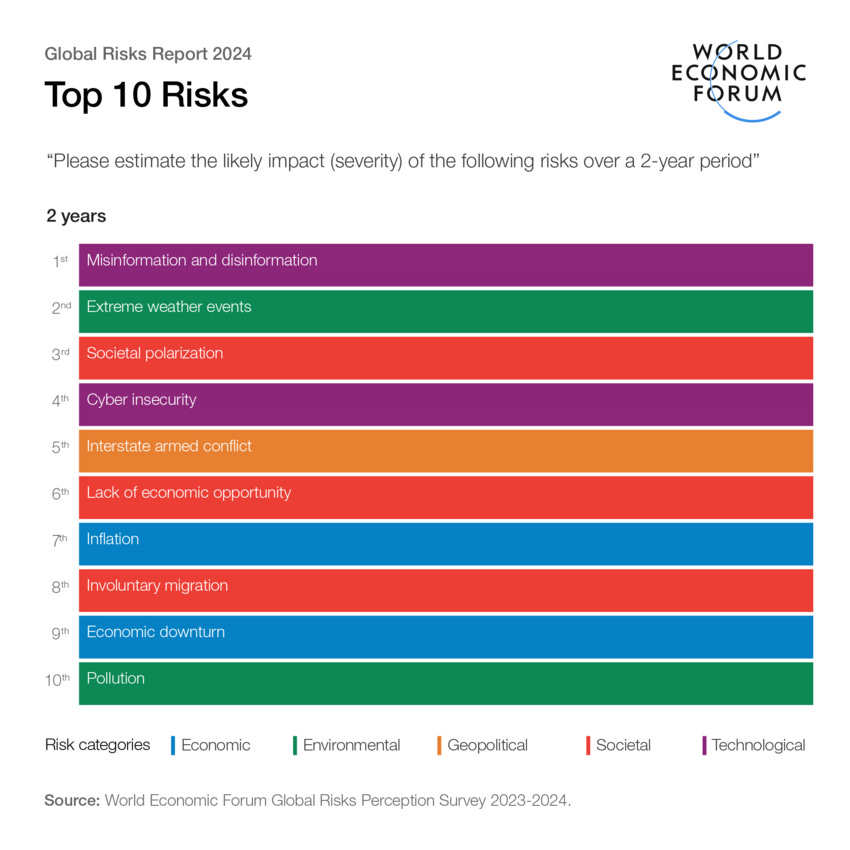
Adding to this complexity is the evolving landscape of infodemics, especially on social media platforms. The arrival of COVID-19 was marked by a significant wave of disinformation fueling an infodemics, but the situation today is arguably more challenging.
Our lab has extensively investigated these processes at the intersection of epidemiology and computational social sciences:
→ Assessing the risks of ‘infodemics’ in response to COVID-19 epidemics
→ The voice of few, the opinions of many: evidence of social biases in Twitter COVID-19 fake news sharing
→ Epidemic proximity and imitation dynamics drive infodemic waves during the COVID-19 pandemic
→ A Public Health Research Agenda for Managing Infodemics: Methods and Results of the First WHO Infodemiology Conference (in collaboration with the WHO)
→ The COVID-19 Infodemics Observatory
Changes in platform policies, particularly on major networks like X/Twitter, have amplified the spread of misleading information, making it increasingly difficult to manage public perception and behavior during health crises. Essentially, it is becoming increasingly difficult, if not impossible, to find reliable fast information sources. At the same time, traditional sources are slower and have to face the fire of denialism that was amplified by the COVID-19 pandemic.
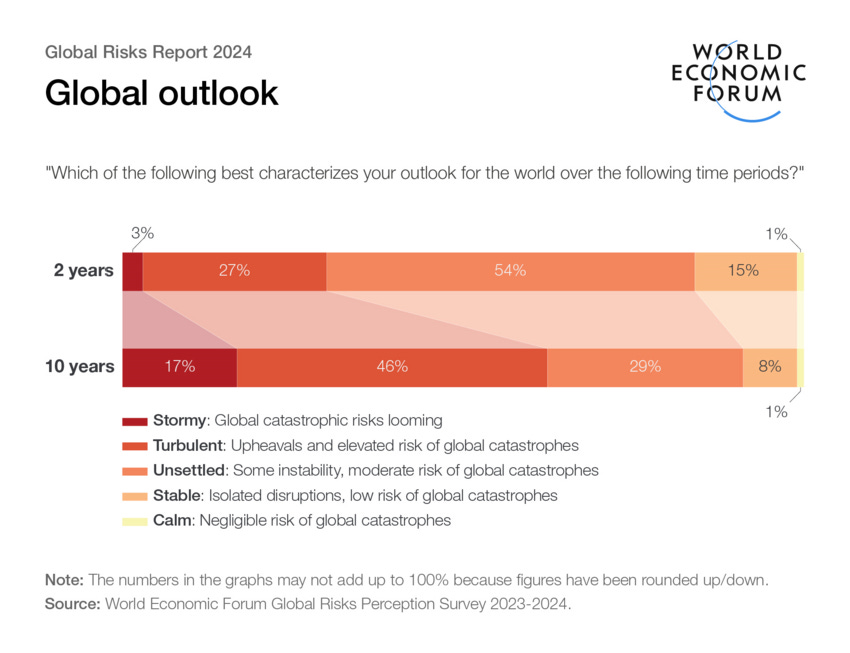
As a result, we now face not only the biological threats of avian flu and mpox but also the social threats posed by infodemics: taken all together, these processes have the potential to destabilize our societies:
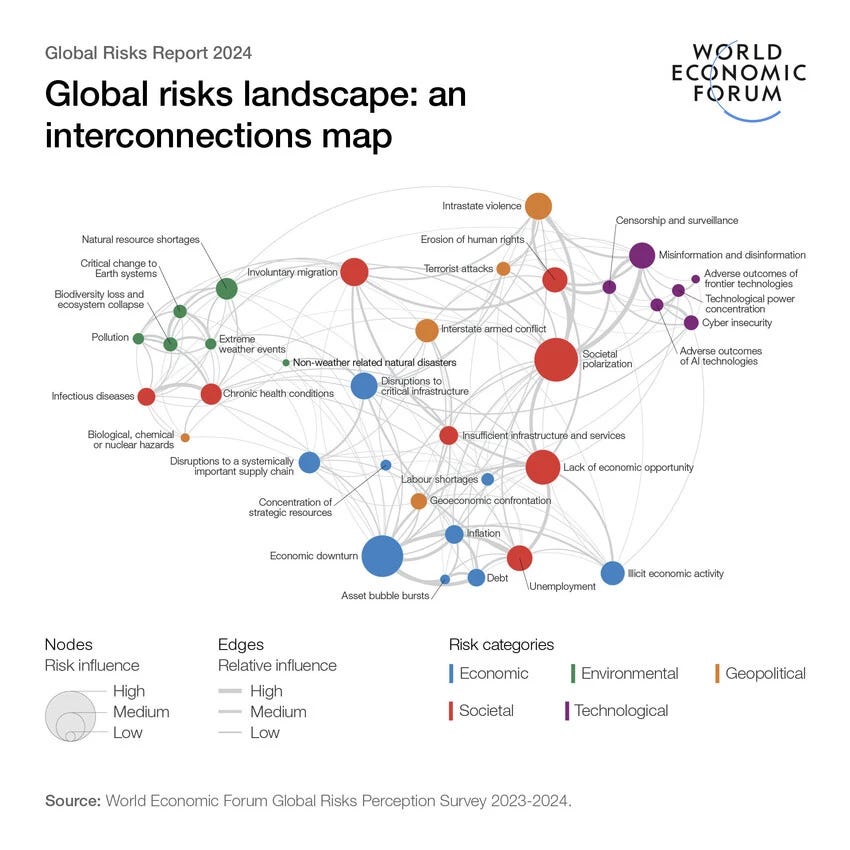
The reason simply relies on the complexity of how the the climate, the environment and our society are interconnected and interdependent:
What’s going on?
Epidemics, in the simplest terms, are outbreaks of infectious diseases that spread rapidly among populations. They differ from pandemics primarily in scale: while an epidemic may affect a large number of people within a particular community or region, a pandemic spreads across countries and continents. The transition from an epidemic to a pandemic depends on several factors, including the nature of the pathogen, the mode and efficiency of transmission, and the response of human populations.
Calling for a PHEIC is a first important step but it does not necessarily mean catastrophic outcomes (such as travel banning, generalized lockdowns and other forms of non-pharmaceutical interventions).
“PHEIC: an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response” — WHO
In fact, during the last 20 years a PHEIC was called for the 2009–2010 H1N1 (or swine flu) pandemic, the 2014 polio declaration, the 2013–2016 outbreak of Ebola in Western Africa, the 2015–2016 Zika virus epidemic, the 2018–2020 Kivu Ebola epidemic, the 2020-2023 COVID-19 pandemic, and the 2022–2023 mpox outbreaks.
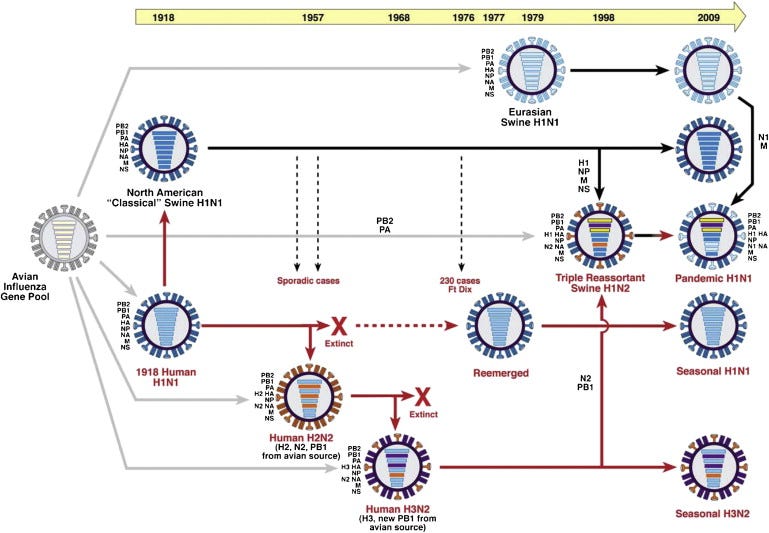
Both avian flu and mpox have zoonotic origins, meaning they are diseases that have jumped from animals to humans. This zoonotic transmission is often facilitated by close contact between humans and animals, whether through the domestication of livestock, wildlife trade, etc. For instance, avian influenza primarily infects birds, but certain strains have evolved to infect mammals, including humans, especially when humans are in close proximity to infected birds or other animals.
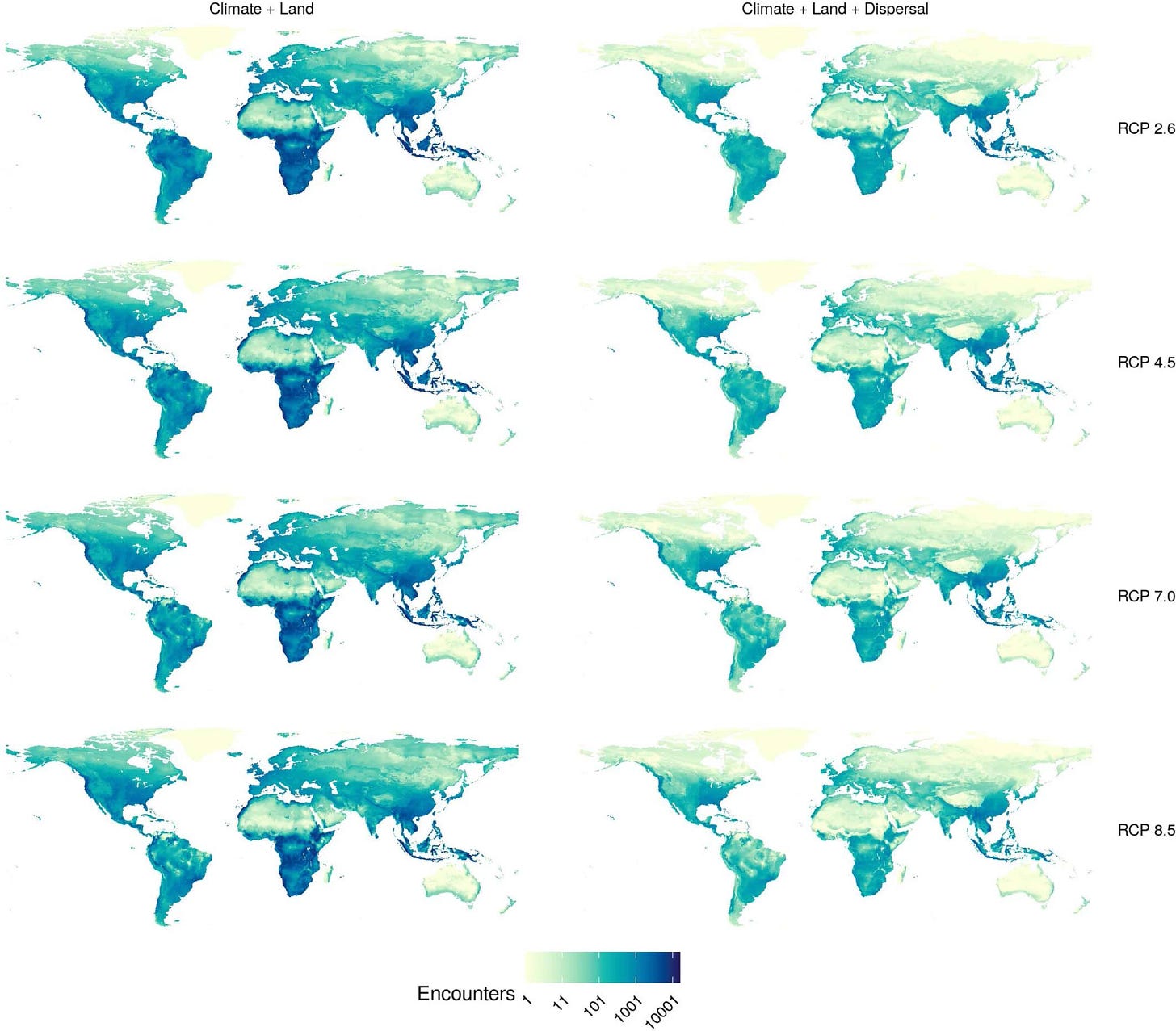
The zoonotic origin of these diseases is intertwined with broader environmental and ecological factors: in fact, climate change plays a significant role by altering ecosystems and driving species into new territories, increasing the likelihood of human-animal interactions. As habitats shrink and animals migrate or adapt to changing environments, the boundaries between human and animal populations blur, creating more opportunities for pathogens to cross species barriers.
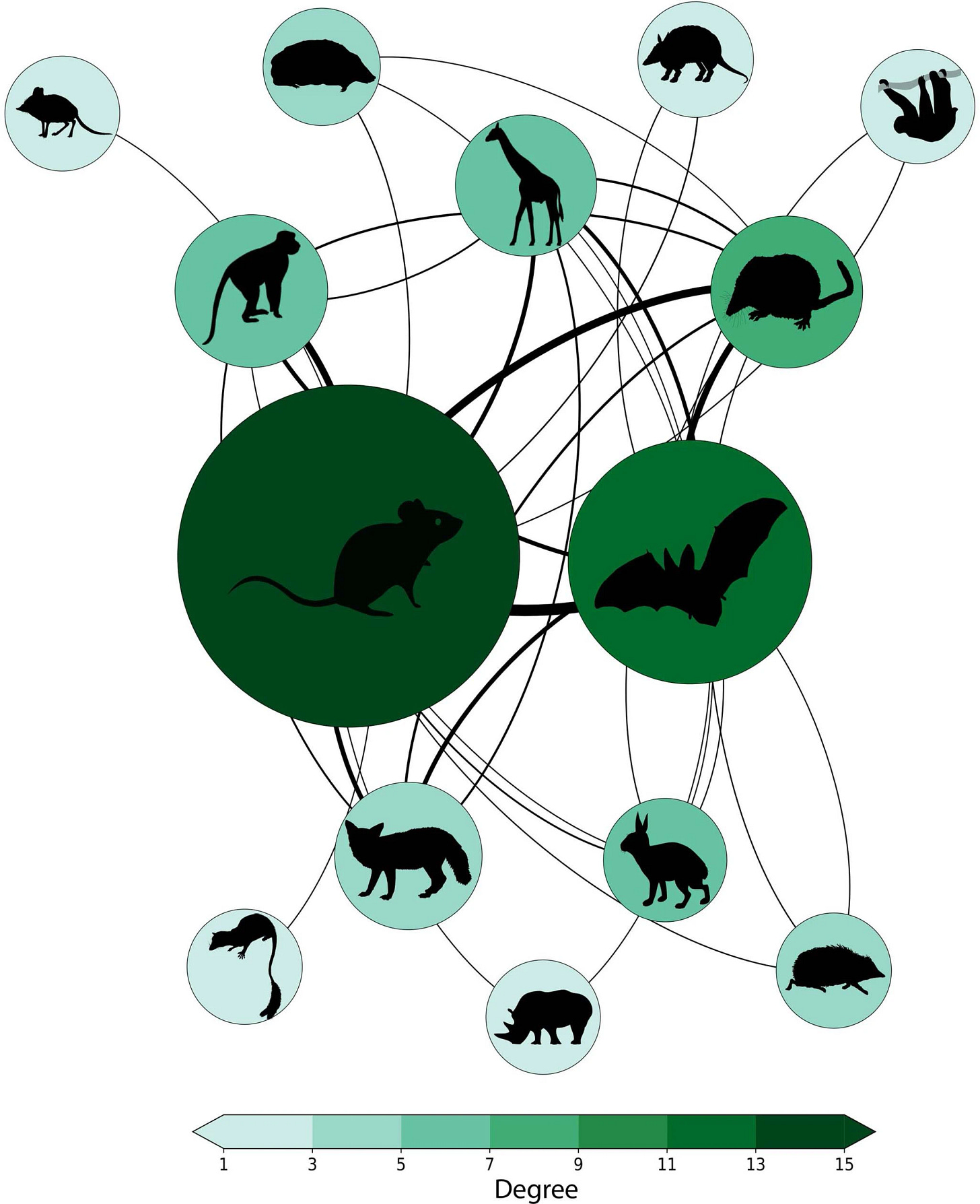
Note, however, that not every zoonotic disease has the potential to become a pandemic: for a pathogen to transition from an epidemic to a pandemic, it must be able to sustain human-to-human transmission on a large scale. This involves a delicate balance of factors, including the pathogen’s ability to replicate and adaptively mutate, the susceptibility of human populations, and the effectiveness of public health measures in containing its spread.
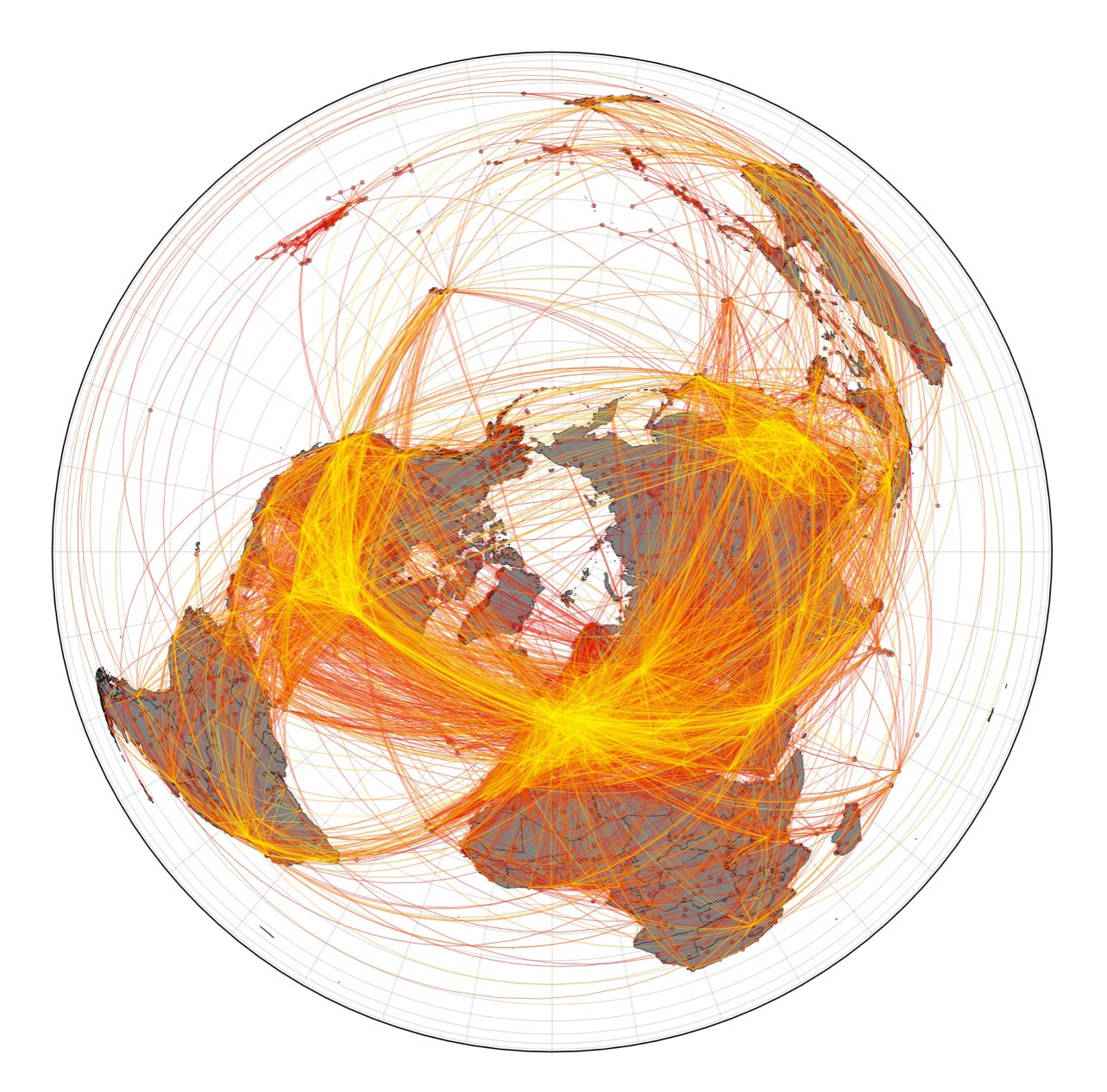
Human mobility and behavior are critical factors in determining the pandemic potential of a disease. In our globalized world, where people and goods move rapidly across borders, an infectious disease can spread far beyond its point of origin in a matter of hours or days. The COVID-19 pandemic provided a stark reminder of how interconnected our world is; a virus that originated in one region quickly became a global threat due to the ease and frequency of international travel:
However, the current situation is further complicated by the pervasive spread of disinformation, particularly on social media platforms. During the COVID-19 pandemic, disinformation undermined public health efforts, fueling skepticism about vaccines, promoting ineffective treatments, and leading to widespread confusion. Today, the problem is even more acute since changes in platform policies, especially on Twitter, have led to a digital environment where misinformation spreads more rapidly and with less oversight. This is concerning, as it unfolds on a population that is already psychologically fatigued from a prolonged pandemic: people are increasingly inclined to ignore or reject public health measures, making it harder to control the spread of (any) disease. This simple fact should not be overlooked.
The potential for concurrent epidemics to evolve into pandemics underscores the interconnectedness of our global systems. Health crises do not exists in isolation: they are part of a larger web of interdependent factors, including economic stability, social cohesion, and environmental sustainability, where risks in one area can have cascading effects across multiple domains, illustrating the complexity of managing global threats.
Infodemics, once again, can exacerbate the impact of a health crisis by polarizing public opinion and undermining trust in health authorities. The psychological weariness of the public, combined with the deluge of conflicting information, fosters tribal behavior, social fragmentation and information centralization. This polarization not only hampers effective public health responses but also has the potential to further destabilize our society by eroding social cohesion and trust in institutions.
This interdependence is a defining characteristic of complex systems, where seemingly isolated events can have far-reaching, unexpected, consequences. In such systems, small disruptions can trigger larger cascades of failures, particularly when the system is already under stress. The interconnected nature of global health, economy, and environment means that we must adopt a systems-thinking approach to anticipate and mitigate the risks of future pandemics.
The key is agility: the faster the response, the more contained the damage.

Still, I can’t see this symbiosis between international organizations and the community of complex systems experts. We have actively collaborated with governments and organizations to provide real-time analyses, modeling and/or projections, but still we lack to be adequately represented in the various boards, such as the GPMB, which are mostly political.
Comparing the epidemiology
Substack does not allow to build tables, AFAIK, therefore I can’t summarize the following information in the best way I hoped for.
COVID-19
Incubation time after exposure: 3-5 days, ranging from 1.8 to 18.8 days. (Source)
Transmission channels:
Airborne: Yes
Droplets: Yes
Surface contact (Fomites): Yes
Sexual transmission: poor/no evidence
Pre-symptomatic transmission: Yes
Asymptomatic transmission: Yes
Recovery time: typically 1-2 weeks, 4-12 weeks or more in severe cases.
Infection Fatality Rate (IFR): typically 0.3-1%, up to 15-20% in elderly or at-risk groups.
Basic Reproductive Number (R0): typically 2-3.5 (original strain), up to 5-8 for variants like Delta.
Vaccine availability and effectiveness: updated monovalent XBB.1.5 vaccine has ~51% effectiveness against infection, 43-52% effectiveness against severe outcomes. (Source)
Bird Flu H5N1
Incubation time after exposure: typically 3-5 days, up to 8 days.
Transmission channels:
Airborne: limited evidence
Droplets: Yes
Surface Contact (Fomites): limited evidence
Sexual Transmission: No
Pre-symptomatic transmission: NA
Asymptomatic transmission: NA
Recovery time: typically 1-4 weeks.
Infection Fatality Rate (IFR): 52% (Source)
Basic Reproductive Number (R0): ~1
Vaccine availability and effectiveness: Stockpiled vaccines based on older strains (A/Vietnam, A/Indonesia) with 60-95% seroconversion rates against new strains. (Source)
Mpox Clade I
Incubation time after exposure: typically 8.5-11.5 days, up to 21 days.
Transmission channels (Source):
Pre-symptomatic transmission: likely negligible. (Source)
Asymptomatic transmission: possible but debated. (Source, Source)
Recovery time: typically 2-4 weeks, up to 4-6 weeks in severe cases.
Infection Fatality Rate (IFR): unknown, CFR up to 11% in some regions (Source, Source)
Basic Reproductive Number (R0): typically 1.2-1.3, up to 1.4-1.6 for specific subclades. (Source)
Vaccine availability and effectiveness: JYNNEOS vaccine: ~66% effectiveness (2 doses), 36% effectiveness (1 dose) against infection; lower effectiveness for post-exposure. (Source, Source, Source)
What do we have to expect?
The dual threat of avian flu and mpox, coupled with infodemics, serves as a stark reminder of the vulnerability of our interconnected world. As societies, we must contend with the reality that we could face multiple, overlapping health crises that strain our healthcare systems, disrupt economies, and challenge social cohesion. The potential impacts of simultaneous pandemics might be deep, affecting every aspect of life from personal health to global security.
In this context, the psychological fatigue from the COVID-19 pandemic cannot be underestimated. Many people are weary of prolonged discussions about public health measures, and this weariness makes them more likely to neglect any recommended precautions. This behavior, combined with the spread of disinformation, creates a dangerous feedback loop where public health measures are ignored or rejected, allowing diseases to spread more easily.
Preparedness and resilience are essential in the face of such complex challenges. Societies need to build adaptive capacities that allow them to respond effectively to emerging threats, whether through robust public health infrastructure, early detection systems, or coordinated international responses. For this reason, the call for PHEIC on mpox is welcome: it is an evidence for a healthy monitoring system.
The experience of COVID-19 has shown that rapid, decisive action can save lives and prevent the worst outcomes of a pandemic. However, these efforts must be supported by clear and consistent communication to fight disinformation and build public trust (or re-build the public trust lost during the last four years).

Global cooperation is essential, as no country can address these challenges alone. The interconnected nature of modern society highlights how health security in one region is linked to the security of others, making international collaboration a cornerstone of pandemic preparedness.
Take home messages
Global interconnectedness: health crises are not singletons, they are linked to economic, environmental, and social systems, requiring a comprehensive, systems-thinking approach.
Communication is key: clear, accurate communication is crucial in managing health crises, as disinformation can have devastating effects.
The enemies are better known than the last one: at variance with COVID-19, who was unexpected, bird flu and mpox are being monitored since a while, with ongoing research on pharmaceutical interventions.
Infodemic threat: don’t forget that disinformation on social media worsens public health challenges, fueling polarization and undermining trust in health authorities.
Need for resilience: we must learn the lessons from COVID-19 pandemic and build adaptive capacities to effectively respond to emerging threats.
Global cooperation essential: international collaboration is fundamental for pandemic preparedness, as health security is a shared global responsibility.